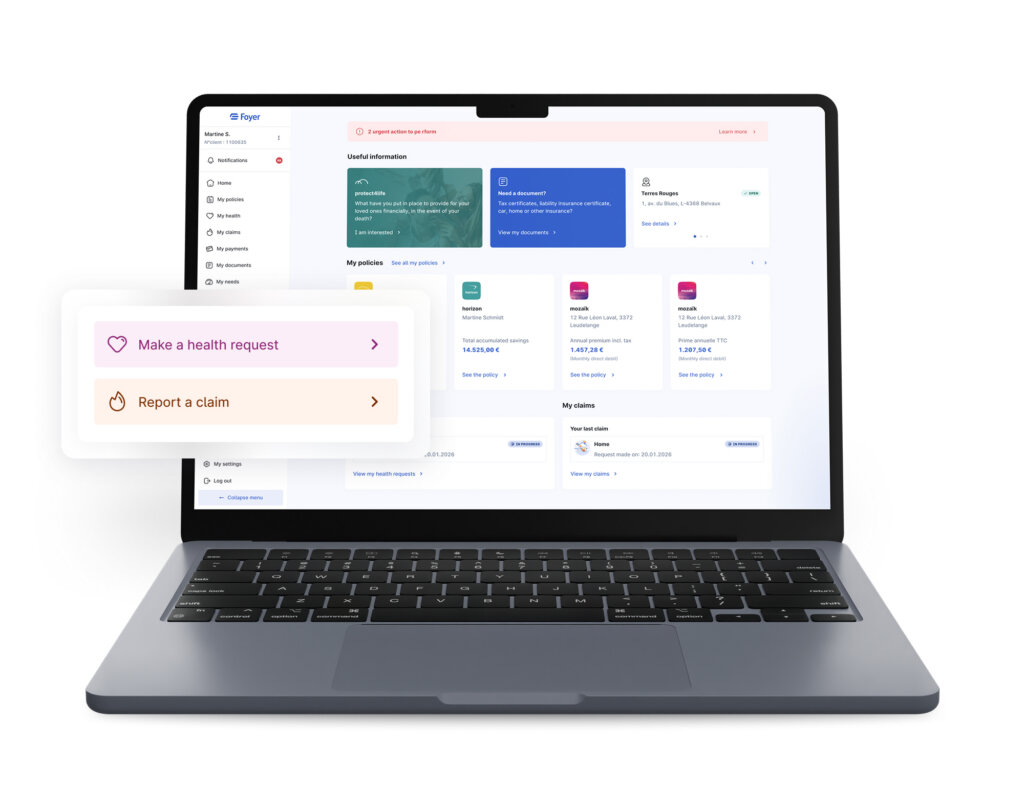
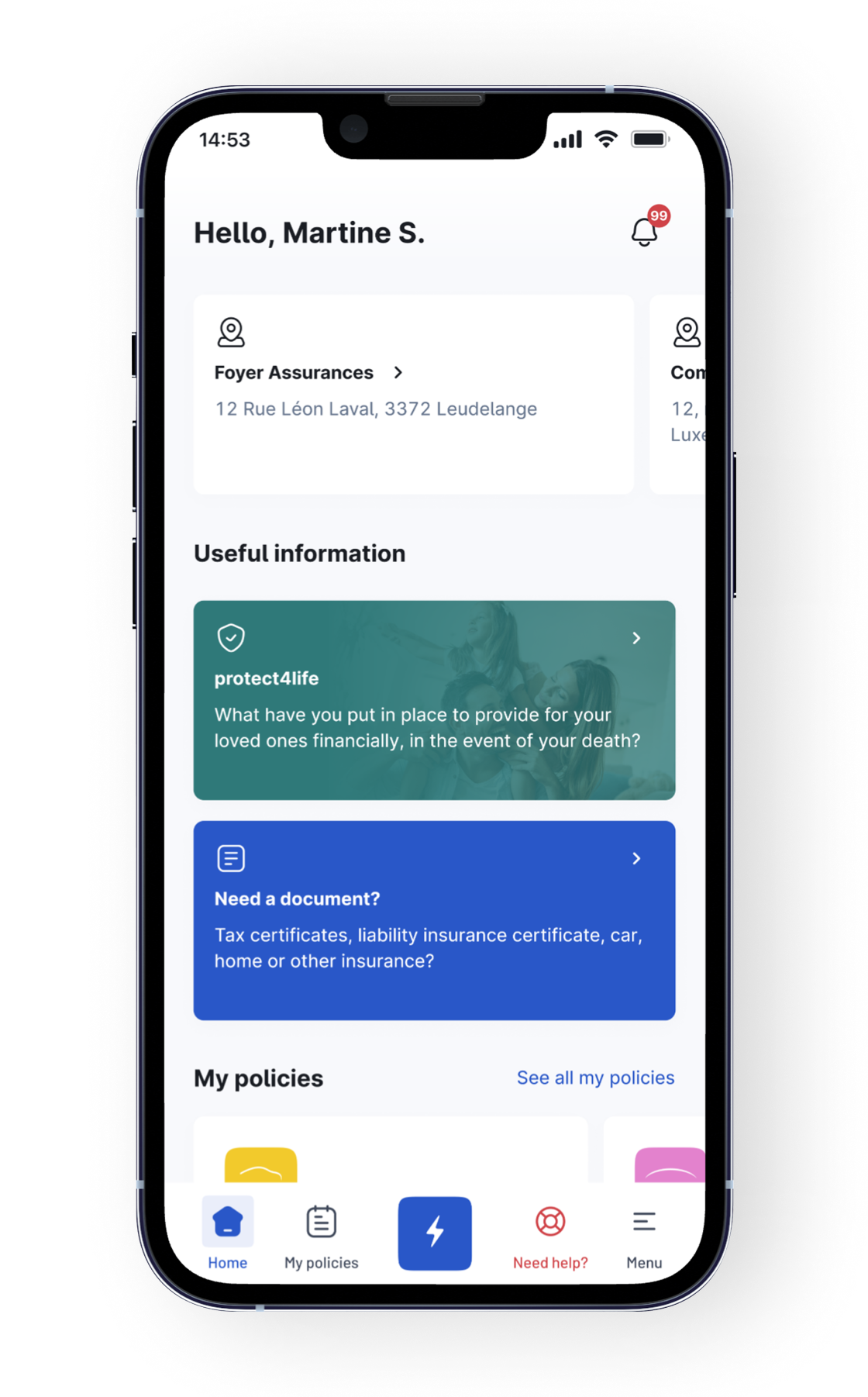
Access your Client Area on your mobile or computer
Available 24/7
We are here to help you 24/7.
Contact your agent
Find their contact details at a glance.
Exclusive services
Save time by reporting claims or submitting requests online.
View your contracts
Easily view the details of your contracts and cover.
SIMPLE + INTUITIVE
Simple and intuitive, MyFoyer makes your online procedures easier
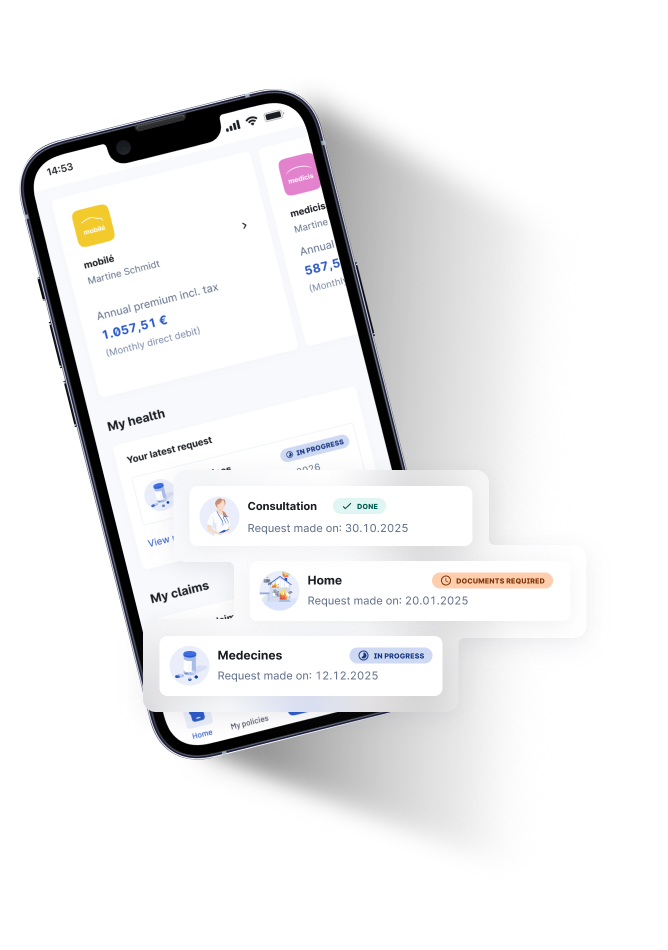
Submit your health and claims requests online
Save time and complete your procedures in your Client Area.
Sign your documents remotely
You can sign your contracts and direct debit authorisations from home.
Real-time tracking
No more waiting around, you can keep track of the progress of your files.
Access your documents
View and download all your important documents.
Manage your profile
Update your personal data yourself.
View and pay your invoices
View and pay your invoices online.
Download the MyFoyer mobile app from the iOS or Android app stores.
Need help? Questions? If you encounter any difficulties, please do not hesitate to contact our customer service team: service-client@foyer.lu
SECURE & FAST
A secure client area that saves you time
Track your reimbursements online
Easily check the status of your reimbursement requests.
Une vue A family overview of all your policiesde tous vos contrats
Find all your contracts and cover, as well as those of your loved ones.
Notifications to keep you informed
Receive alerts when new reimbursements, documents or required actions are available.
A secure space for your communications
Track or submit new requests, contact your agent. It’s simple and secure.